Volunteers of America (VOA) is one of the nation’s largest and most established human services organizations, reaching more than 2 million people annually across 47 states, Washington, D.C., and Puerto Rico. With a mission rooted in supporting the most vulnerable, we deliver critical services in housing, behavioral health, reentry, and social support – often serving individuals facing complex, overlapping barriers to care.
A key component of our work is VOA’s growing Community Health Worker (CHW) workforce. Often recruited from the very communities they serve, CHWs are uniquely positioned to build trust, navigate local systems, and advocate for client needs that extend far beyond the walls of a clinic. From securing stable housing to accessing food assistance and health coverage, CHWs act as vital bridges between underserved populations and the services that support long-term well-being.
Yet despite their critical role, many CHWs lack access to the tools needed to efficiently track client progress, coordinate referrals, and demonstrate outcomes. That’s why VOA partnered with Dimagi – to close this gap and equip our CHW workforce with a robust, low-code case management platform built on CommCare. This collaboration is designed to strengthen VOA’s ability to address Social Determinants of Health (SDoH) for vulnerable populations at scale while ensuring that CHWs can focus more on client engagement and less on administrative burden.
Addressing the Root Causes of Health Disparities with the CHW Model
Access to healthcare is about more than just doctor’s visits – it’s about addressing the everyday challenges that prevent people from staying engaged in their care. For many, challenges like unstable housing, food insecurity, lack of reliable transportation, and limited health literacy can prevent even the most basic access to services. Traditional healthcare systems are often ill-equipped to address these deeply rooted social and structural barriers.
This is where Community Health Workers (CHWs) play a transformative role. As trusted members of the communities they serve, CHWs provide culturally responsive support, help clients navigate complex social and healthcare systems, connect to critical services, and advocate for their needs in ways that traditional providers often cannot.
At VoA, we’re leveraging CHWs as a key solution to addressing Social Determinants of Health (SDoH), and other non-medical factors that profoundly shape health outcomes. With a focus on behavioral health, housing, and wraparound social services, we empower CHWs to support individuals facing compounding vulnerabilities. Now, with support from Public Health AmeriCorps, we’re expanding our CHW workforce and investing in digital tools that enhance care coordination, streamline service delivery, and amplify the impact of our field teams.
The communities we serve face some of the most persistent barriers to care:
- Unstable Housing: Without secure shelter, clients struggle to maintain health routines, store medications, or attend follow-up appointments.
- Food Insecurity: Limited access to nutritious food exacerbates chronic conditions and undermines overall well-being.
- Transportation Gaps: Many clients live in areas with limited access to reliable transit, making it difficult to access care or fill prescriptions.
- Health Literacy: Understanding treatment plans, insurance paperwork, and social services can be overwhelming without guidance.
As we scaled our CHW program with support from a Public Health AmeriCorps grant, we faced a critical operational hurdle: our legacy case management system carried high recurring costs and was ill-suited to the needs of a mobile, non-technical workforce. To ensure long-term sustainability and better support for frontline teams, we sought a modern, user-centered digital solution.
Transforming Service Delivery Through Digital Enablement
With a growing CHW workforce embedded directly in communities across the country, we’re reimagining how care and support are delivered to those facing complex health and social needs. As part of our Public Health AmeriCorps-funded expansion, we recognized the need for a digital infrastructure that could adapt to local contexts, reduce administrative overhead, and support real-time coordination among field staff.
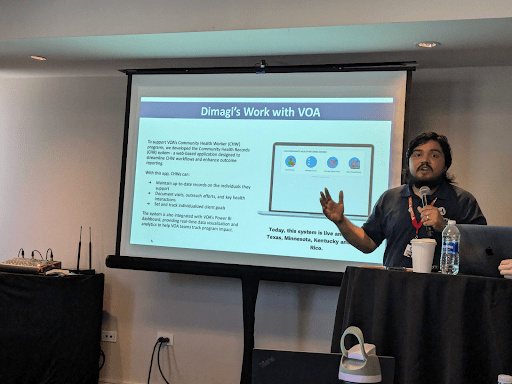
To meet this need, we partnered with Dimagi to implement CommCare, a HIPAA-compliant, low-code case management platform built specifically for frontline teams. This solution has enabled has enabled 30 CHWs across Puerto Rico, Minnesota, Texas and Kentucky to:
- Securely record demographic, medical history, and service needs
- Complete structured assessments related to social drivers of health, such as housing stability, food access, transportation availability, behavioral health needs, and social connectedness
- Track client goals, interventions, and follow-ups
- Generate real-time reports and integrate with VOA’s PowerBI system for deeper insights
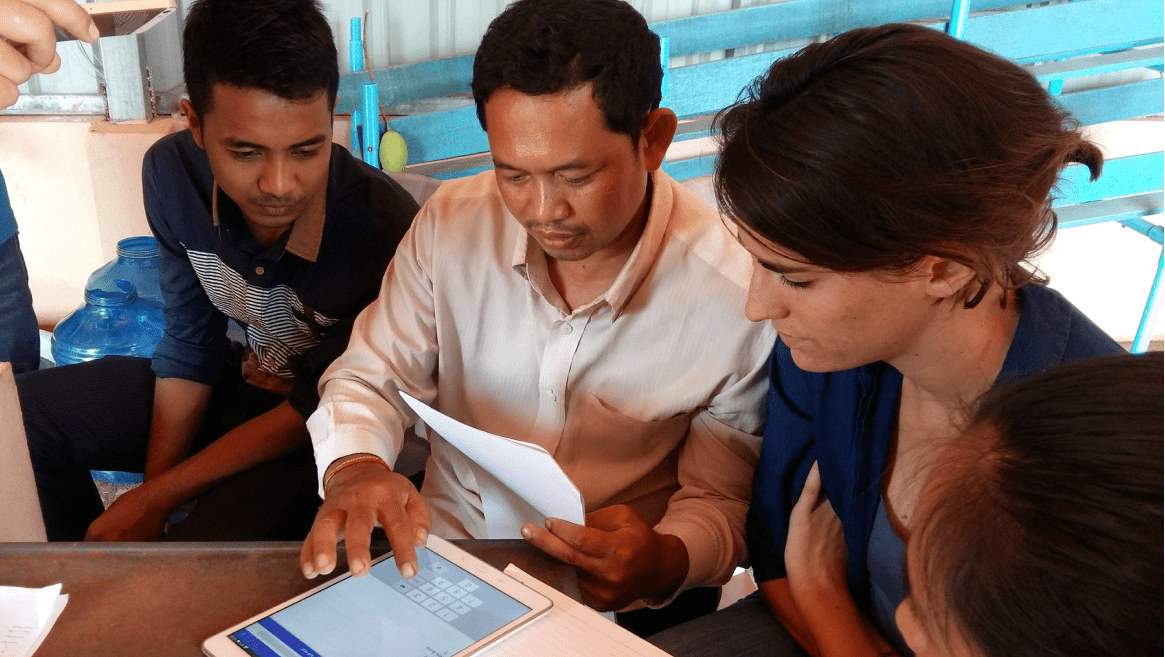
This digital solution is designed to meet the realities of CHW work in fast-paced, high-need settings. With CommCare’s intuitive, mobile-friendly interface, CHWs can efficiently document and access client information in the field – no technical background required. By streamlining data entry and reducing administrative overhead, the platform enables CHWs to devote more time to what matters most: building relationships, coordinating care, and advocating for the people we serve.
The implementation followed a focused three-month timeline, designed to ensure the system was responsive to CHW needs and grounded in real-world use. Key phases included:
- User interviews & discovery to align the system with CHW needs
- Configuration & testing of a Minimum Viable Product (MVP)
- Training & onboarding support to ensure a seamless rollout
- Post-live stabilization & refinement based on user feedback
Several CHWs from Puerto Rico shared that the system is easy to use, intuitive, and helps them stay on top of their clients’ progress and goals. This frontline perspective echoes the sentiment shared by Alberto Maldonado, Regional Director at VOA Puerto Rico, who emphasized the importance of data systems in a recent LinkedIn post:
“In my line of work, I don’t just collaborate with frontline staff – I also focus on connecting services with providers and people, ensuring that all stakeholders are aligned, needs are met, and goals are achieved. Strengthening data collection systems is key to delivering quality, sustainable community services.”
Charting the Future of CHW Programs
Even as we expand our CHW program’s reach and impact, broader systemic challenges persist. CHW programs across the country continue to face high turnover, fragmented funding streams, and limited access to sustainable reimbursement mechanisms through public and private insurance – barriers that threaten the long-term viability of community-based care models.
While technology is a powerful enabler, addressing the broader challenges facing CHW programs will require a multifaceted approach – one that includes continued investment, supportive policy frameworks, and collaboration across sectors. Through our partnership with Public Health AmeriCorps, we’re not only strengthening our own CHW infrastructure but also contributing to the growing recognition of CHWs as essential partners in advancing health equity, prevention, and community-centered care.
As part of this effort, VOA and Dimagi are committed to sharing learnings with the broader field – co-presenting at industry conferences and public health forums, engaging in peer learning networks, and sharing insights on how digital tools can extend CHW capacity, strengthen data-driven decision-making, and support community impact.
With continued momentum, CHW programs like ours offer a compelling model for transforming health systems from the ground up – one that honors lived experience, prioritizes relationships, and ensures that the path to better health is rooted in the realities of everyday life.